“Helping someone find their words for the first time, or be able to eat after a stroke is so rewarding. I am reminded each day that these things that we all take for granted are fragile.”
– Laddie Erbele, speech language pathologist
A stroke, a traumatic brain injury, a neurological condition … those are the kinds of life-altering events that bring people to Laddie Erbele’s world. Her job and her joy are helping them relearn the skills to get them where they can function and live life to their fullest potential.
“The very best reward is when we have our reunions and our patients come up to us and are unrecognizable because they have progressed so far. To see people well and whole after they had felt so devastated is truly beyond words.”
– Laddie Erbele, speech language pathologist
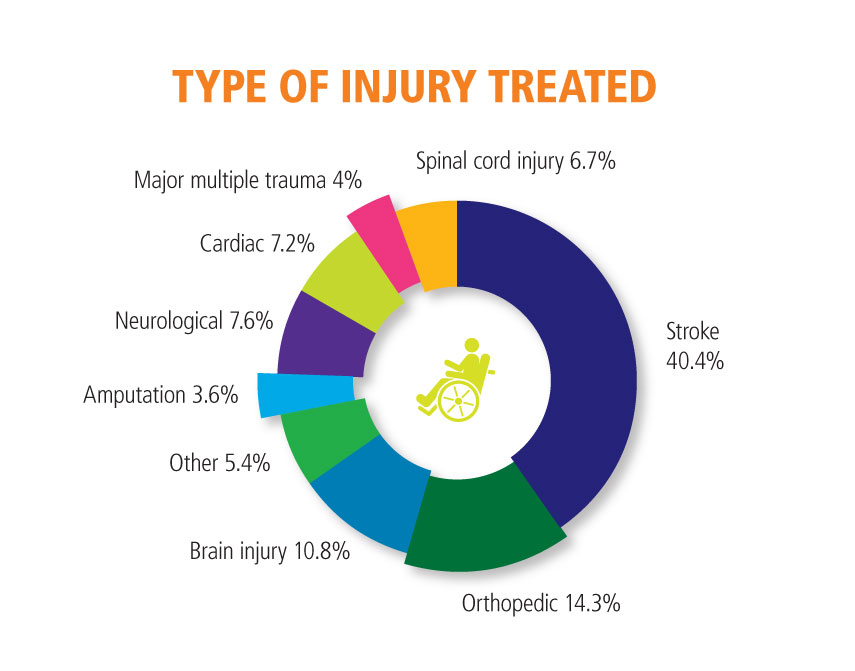
Laddie Erbele is a speech and language pathologist at Community Hospital’s William R. Lewis, MD, Inpatient Rehabilitation Unit (IRU). The unit provides rehabilitation services to individuals who have suffered an acute illness, injury, or accident, resulting in significant functional decline.
The IRU team
❙ Physiatrists
❙ Rehabilitation nurses
❙ Physical, occupational, and speech-language therapists
❙ Social workers
❙ Clinical dietitians
❙ Doctor of osteopathic medicine
❙ The other team — your family
Family is a major support system. The IRU includes
them in treatment, education, and planning throughout
a patient’s stay.
A team that works well together results in happier,
healthier patients.
The majority of IRU patients are able to return to their
homes after making significant gains in their life skills.
chomp.org/iru